Colon and rectal cancer, often grouped together as colorectal cancer, presents a significant health concern worldwide. Early detection through screening is crucial for effective treatment and improved survival rates. However, the timing of when to initiate screening can be perplexing due to varying guidelines and individual risk factors. This article aims to clarify the appropriate age to begin colorectal cancer screening, explore the available screening methods, and underscore the importance of early detection.
Understanding Colorectal Cancer
Colorectal cancer originates in the colon or rectum, parts of the digestive system. It typically begins as benign growths called polyps, which can evolve into cancer over time. Screening plays a pivotal role in identifying these polyps early or detecting cancer in its initial stages, when treatment outcomes are most favorable.
Why Screening is Critical
Screening for colorectal cancer is crucial for several reasons:
- Early Detection: Identifying cancer early significantly enhances the chances of successful treatment and survival.
- Prevention: Screening can detect and remove polyps before they become cancerous.
- Reduced Mortality: Regular screening has been shown to decrease mortality rates associated with colorectal cancer.
Recommended Age to Initiate Screening
The age at which individuals should begin colorectal cancer screening depends on various factors, including age, family history, and overall risk profile. Here are the general recommendations:
- Average-Risk Individuals: Most guidelines suggest starting screening at age 45. This adjustment from the previous guideline of age 50 reflects the rising incidence of colorectal cancer among younger adults.
- High-Risk Individuals: Those with increased risk factors may need to commence screening earlier and undergo more frequent screenings. High-risk factors include:
- Personal history of inflammatory bowel disease (e.g., Crohn’s disease or ulcerative colitis).
- Genetic syndromes like Lynch syndrome or familial adenomatous polyposis (FAP).
Screening Methods
Several effective screening tests are available for detecting colorectal cancer, each with its advantages and limitations:
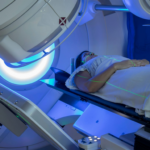
- Colonoscopy: This procedure is widely regarded as the preferred method for colorectal cancer screening. It involves examining the entire colon and rectum using a flexible tube with a camera. During a colonoscopy, polyps and abnormal tissues can be identified and removed. It is typically recommended every 10 years for average-risk individuals.
- Flexible Sigmoidoscopy: Similar to a colonoscopy but only examines the lower portion of the colon and rectum. It is less invasive but may miss abnormalities in the upper colon. Recommended every 5 years.
- Fecal Immunochemical Test (FIT): This non-invasive test detects hidden blood in the stool, which can indicate the presence of cancer. It is easy to perform at home and is recommended annually.
- Fecal Occult Blood Test (FOBT): Another stool-based test that checks for blood. It necessitates dietary limitations before the test and is advised once a year.
- Stool DNA Test (Cologuard): This test examines stool samples for specific DNA mutations and blood. It can be performed at home and is recommended every 3 years.
- CT Colonography (Virtual Colonoscopy): A specialized CT scan that provides detailed images of the colon and rectum. Recommended every 5 years.
Determining the Right Time for Screening
The decision on when to start screening should be a collaborative discussion between individuals and their healthcare providers, taking into account personal risk factors and family medical history. Specific recommendations based on risk categories include:
- Average-Risk Individuals: Initiate screening at age 45 and continue regular screenings until age 75. For individuals aged 76 to 85, the decision to continue screening should be based on individual health status, life expectancy, and prior screening history.
- High-Risk Individuals:
- Family History: Begin screening at age 40 or 10 years earlier than the youngest age at diagnosis of a first-degree relative (parent, sibling, or child), whichever is earlier.
- Genetic Syndromes: Start screening in the teens or twenties, as recommended by healthcare providers for conditions like Lynch syndrome or FAP.
- Personal Health Conditions: Individuals with inflammatory bowel disease should discuss screening timing and frequency with their doctors, potentially starting earlier and undergoing more frequent tests.
Lifestyle and Risk Reduction
In addition to regular screening, certain lifestyle modifications can help reduce the risk of colorectal cancer:
- Diet: Maintain a diet rich in fruits, vegetables, and whole grains, while limiting red and processed meats.
- Exercise: Engage in regular physical activity.
- Alcohol and Tobacco: Limit alcohol consumption and avoid smoking.
Colorectal cancer screening is indispensable for early detection and prevention of this prevalent cancer. Starting screening at the appropriate age and adhering to regular testing schedules can significantly mitigate the risk of advanced cancer and enhance survival rates. Individuals are encouraged to discuss their unique risk factors with healthcare providers to determine the most suitable screening strategy.
Summary
Determining the optimal time to commence colorectal cancer screening is pivotal for effective prevention and early intervention. For average-risk individuals, screening typically begins at age 45, whereas those at higher risk may initiate earlier. Various screening methods, including colonoscopy, FIT, and stool DNA tests, offer diverse benefits. Consulting with a healthcare provider regarding personal and familial medical history can facilitate the development of an optimal screening plan.